
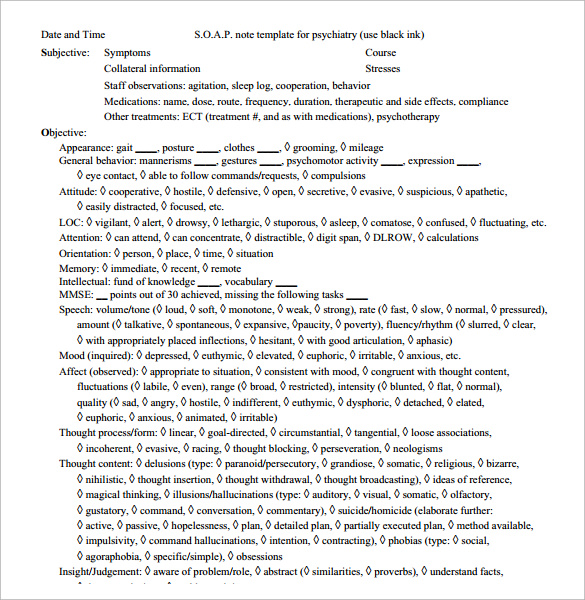
SOAP notes provide a concise and standardized way to document patient care, making them an essential tool for busy healthcare professionals. The assessment is a summary of the patient's condition, and the plan outlines the next steps in their care. They then move on to objective observations, such as vital signs and physical examination findings. SOAP notes begin with a description of the patient's symptoms, as well as any relevant medical history. The acronym stands for Subjective, Objective, Assessment, and Plan. SOAP notes are a common method used by healthcare professionals to document patient care. We'll also provide some tips on creating an effective documentation system for your practice.
SOAP NOTES HOW TO
In this blog post, we will discuss how to write massage therapy SOAP notes, as well as provide some examples. They allow you to track the progress of your clients, as well as provide information to insurance companies and other professionals. SOAP notes are a standard way of documenting massage therapy sessions. This can be a difficult task, especially when you're taking care of multiple clients during a single session. Geeky Medics accepts no liability for loss of any kind incurred as a result of reliance upon the information provided in this video.Are you a massage therapist who struggles to write effective SOAP notes after or during patient massage appointments? If so, you're not alone. DO NOT perform any examination or procedure on patients based purely on the content of these videos. Join the Geeky Medics community: 👩👩👧👧Īlways adhere to medical school/local hospital guidelines when performing examinations or clinical procedures. Subscribe to our newsletter to be the first to know about our latest content: ✉️ You can access a range of psychiatry OSCE stations here: Ĭheck out our other awesome clinical skills resources including: This video demonstrates how to perform a mental state examination (MSE) on a patient exhibiting features of anxiety in the context of a psychiatry OSCE station.Īccess our step-by-step MSE written guide alongside the video here:
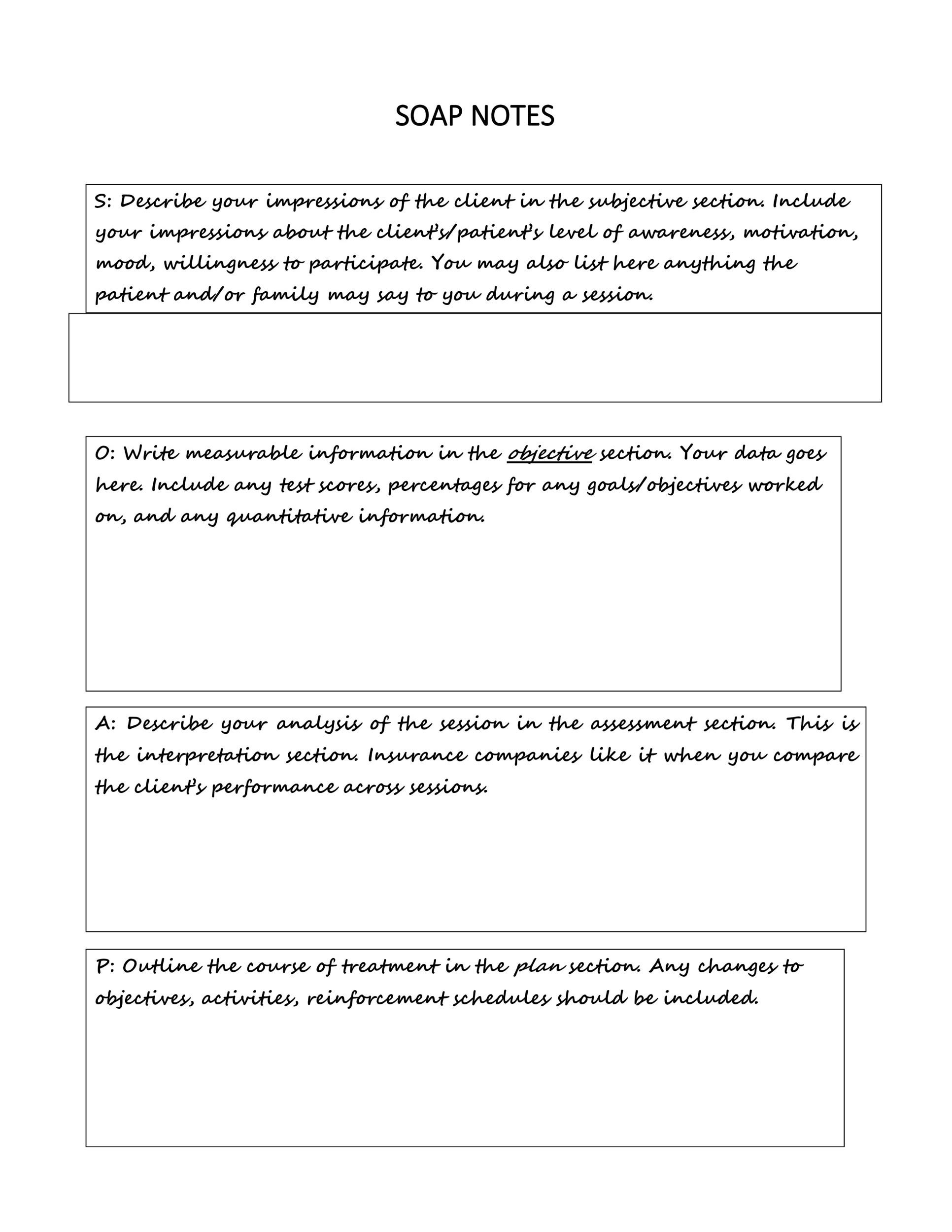
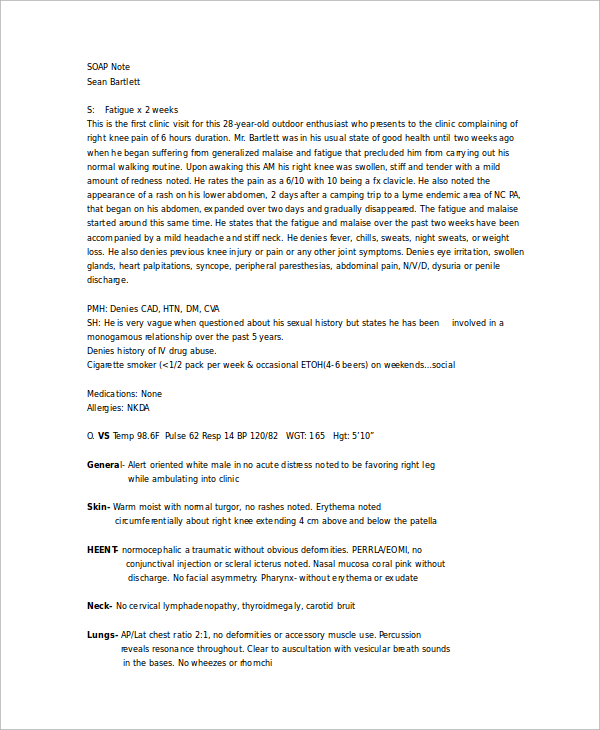
“Impression: community-acquired pneumonia”.“Chest X-ray revealed increased opacity in the right lower zone, consistent with consolidation”ĭocument your impression of the diagnosis (or differential diagnosis):.“Raised white cell count (15) and CRP (80)”.“Tachypnea (respiratory rate 22) and hypoxia (SpO 2 87% on air)”.The assessment section is where you document your thoughts on the salient issues and the diagnosis (or differential diagnosis), which will be based on the information collected in the previous two sections. Some examples of investigation results include: “There were no cranial nerve deficits noted.”.“Widespread expiratory wheeze on auscultation of the chest.”.Some examples of clinical examination findings may include: Temperature (including any recent fevers)Īn assessment of the patient’s fluid intake and output including:.SpO 2 (also document supplemental oxygen if relevant).“The patient appeared to be very pale and in significant discomfort.”). Objective observations Appearanceĭocument the patient’s appearance (e.g. The objective section needs to include your objective observations, which are things you can measure, see, hear, feel or smell. You might also be interested in our OSCE Flashcard Collection which contains over 2000 flashcards that cover clinical examination, procedures, communication skills and data interpretation.


 0 kommentar(er)
0 kommentar(er)
